A new biomarker for blood–brain barrier dysfunction in Alzheimer's disease
Summary Text
APOE ɛ4, a major risk factor for Alzheimer's disease (AD), directly impairs the blood–brain barrier (BBB). This study aimed to verify the influence of APOE ɛ4 on the BBB clearance function, estimated with an advanced magnetic resonance diffusion-prepared arterial spin labeling (DP-ASL) technique. We believe that our study makes a significant contribution in this field because an improved understanding of APOE ɛ4-related pathophysiology will aid the development of novel therapeutic strategies for AD.
Full text
Alzheimer’s disease (AD) is the most common type of dementia. An etiology of AD would be excessive accumulation of toxic forms of β-amyloid (Aβ), assumed to result from an imbalance between its production and clearance. Individuals with early-onset AD-related gene mutations show both increased production and decreased clearance of Aβ, whereas those with late-onset AD, which accounts for > 95% of cases, exhibit only decreased Aβ clearance.
The ε4 allele of APOE gene is the strongest and most validated genetic risk factor for late-onset AD. Previous research has shown that carrying one APOE ε4 allele (heterozygotes) increases the risk of late-onset AD 3–4-fold, and carrying two APOE ε4 alleles (homozygotes) increases the risk 9–15-fold. Considering the prevalence and risk-determining effect, an improved understanding of APOE ɛ4-related pathophysiology will aid the development of novel therapeutic strategies for late-onset.
Emerging evidence suggests that APOE ɛ4 directly impairs the blood–brain barrier (BBB), a highly selective semipermeable border formed by capillary endothelial cells, astrocytic end-feet, and pericytes. Astrocyte-secreted ApoE4 induces the degeneration of brain capillary pericytes that maintain BBB integrity, and individuals carrying APOE ɛ4 show BBB dysfunction leading to cognitive decline, independent of AD pathology.
The current study aimed to verify the influence of APOE ɛ4 on effective BBB clearance, evaluated using an advanced magnetic resonance diffusion-prepared arterial spin labeling (DP-ASL) technique. An appealing feature of the DP-ASL technique is its non-invasive nature and ability to quantitatively estimate water exchange rate across the BBB (kw index) using a conventional 3.0-T MRI system.
First, we presented the clinical characteristics and neuropsychological scores for APOE ɛ4 noncarrier, heterozygous, and homozygous groups from the early stages of the Alzheimer's continuum cohort. Second, we compared AD-related imaging biomarkers, including the BBB kw map, quantitative susceptibility mapping (QSM), [11C]Pittsburgh compound B-positron emission tomography (PiB-PET), and cortical thickness. Finally, we assessed the correlation of kw values with neuroimaging metrics of AD pathology and neuropsychological scores. We concluded that APOE ɛ4 dose would be associated with poor brain-waste clearance through the BBB, causing brain iron and Aβ accumulation.
Reference
10.1136/jnnp-2021-328519
The ε4 allele of APOE gene is the strongest and most validated genetic risk factor for late-onset AD. Previous research has shown that carrying one APOE ε4 allele (heterozygotes) increases the risk of late-onset AD 3–4-fold, and carrying two APOE ε4 alleles (homozygotes) increases the risk 9–15-fold. Considering the prevalence and risk-determining effect, an improved understanding of APOE ɛ4-related pathophysiology will aid the development of novel therapeutic strategies for late-onset.
Emerging evidence suggests that APOE ɛ4 directly impairs the blood–brain barrier (BBB), a highly selective semipermeable border formed by capillary endothelial cells, astrocytic end-feet, and pericytes. Astrocyte-secreted ApoE4 induces the degeneration of brain capillary pericytes that maintain BBB integrity, and individuals carrying APOE ɛ4 show BBB dysfunction leading to cognitive decline, independent of AD pathology.
The current study aimed to verify the influence of APOE ɛ4 on effective BBB clearance, evaluated using an advanced magnetic resonance diffusion-prepared arterial spin labeling (DP-ASL) technique. An appealing feature of the DP-ASL technique is its non-invasive nature and ability to quantitatively estimate water exchange rate across the BBB (kw index) using a conventional 3.0-T MRI system.
First, we presented the clinical characteristics and neuropsychological scores for APOE ɛ4 noncarrier, heterozygous, and homozygous groups from the early stages of the Alzheimer's continuum cohort. Second, we compared AD-related imaging biomarkers, including the BBB kw map, quantitative susceptibility mapping (QSM), [11C]Pittsburgh compound B-positron emission tomography (PiB-PET), and cortical thickness. Finally, we assessed the correlation of kw values with neuroimaging metrics of AD pathology and neuropsychological scores. We concluded that APOE ɛ4 dose would be associated with poor brain-waste clearance through the BBB, causing brain iron and Aβ accumulation.
Reference
10.1136/jnnp-2021-328519
| Title | APOE ɛ4 dose associates with increased brain iron and β-amyloid via blood–brain barrier dysfunction |
| Author | Yuto Uchida, Hirohito Kan, Keita Sakurai, Yoshihiko Horimoto, Emi Hayashi, Akihiko Iida, Nobuyuki Okamura, Kenichi Oishi, Noriyuki Matsukawa |
| Article URL | https://jnnp.bmj.com/content/early/2022/04/28/jnnp-2021-328519.abstract |
Representative images
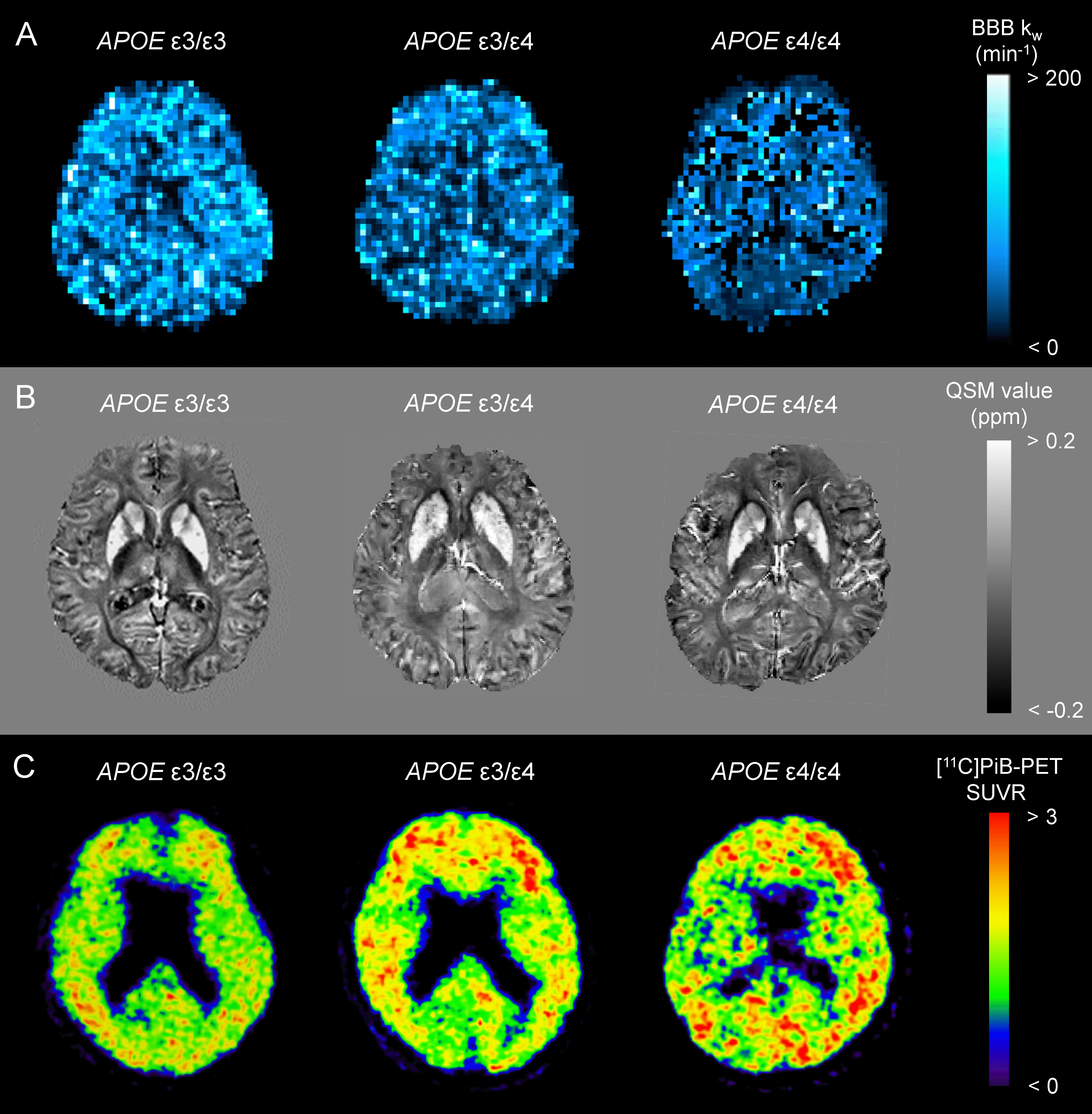
BBB kw map (A), QSM (B), and [11C]PiB-PET SUVR (C) from an APOE ɛ4 noncarrier (ε3/ε3), a heterozygote (ε3/ε4), and a homozygote (ε4/ε4) are displayed.